 Providing Related Services to Homebound Students Survey Results
Providing Related Services to Homebound Students Survey Results
During the last quarter of 2017, Your Therapy Source posted a survey on providing related services to homebound students. A school-based therapist submitted a question regarding how other districts were providing related services to students who remain at home, therefore a survey was created to see how other districts service homebound students. It was requested to only answer the survey if you are a related service provider working in a school district (preschool or K-12). The survey received 238 responses.
Results of Providing Related Services to Homebound Students Survey:
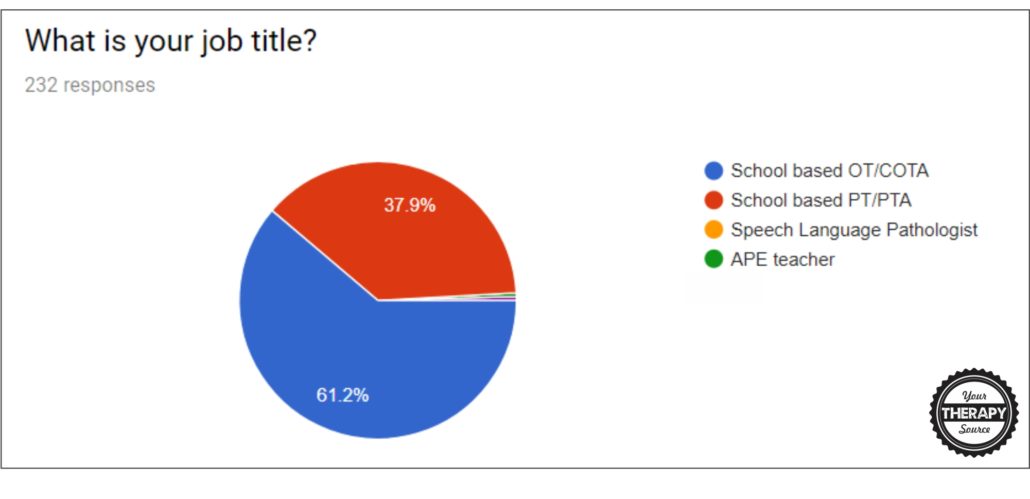
Question 1: What is your job title?
- 61.2% were OT/COTAs
- 37.9% were PT/PTAs
- the remaining responders were 1 SLP and 1 APE teacher
Question #2: Do the majority of your school district’s homebound students receive physical, occupational or speech therapy as direct or consult services?
- 54% received direct services
- 30.2% received consult services
- 3% do not provide services to homebound students

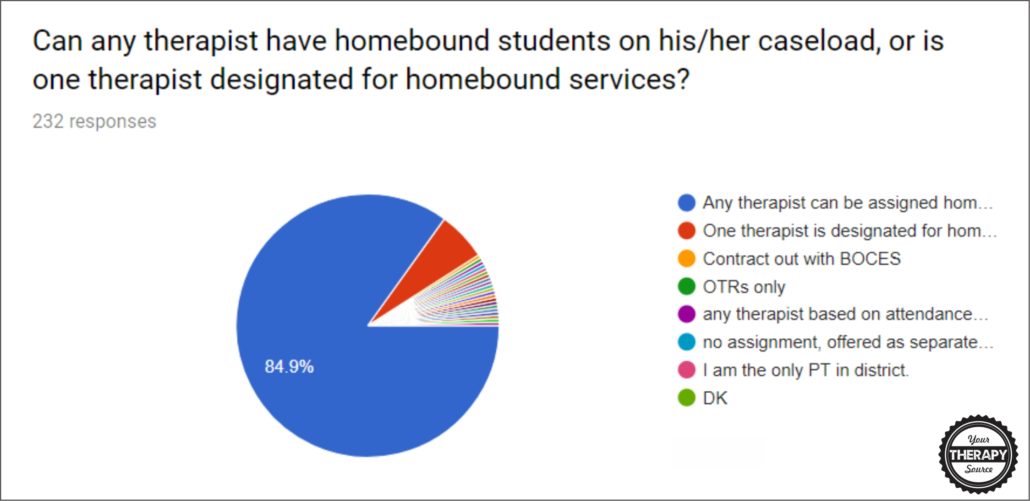
Question #4: Can any therapist have homebound students on his/her caseload, or is one therapist designated for homebound services?
- 84.9% any therapist
- 6% one therapist is designated
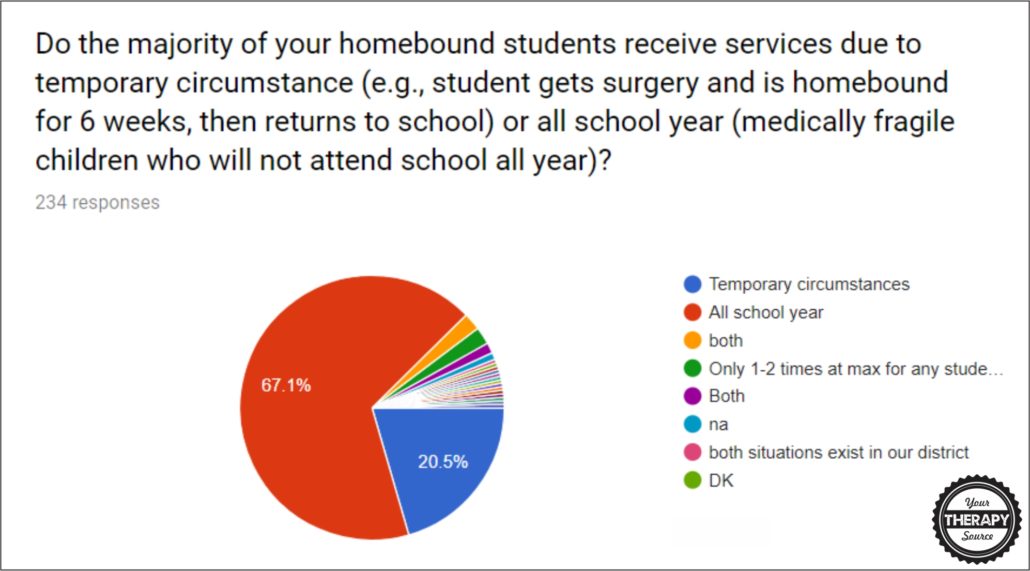
Question #5: Do the majority of your homebound students receive services due to temporary circumstance (e.g., student gets surgery and is homebound for 6 weeks, then returns to school) or all school year (medically fragile children who will not attend school all year)?
- 67.1% homebound students receive related services all school year
- 20.5% are temporary circumstances
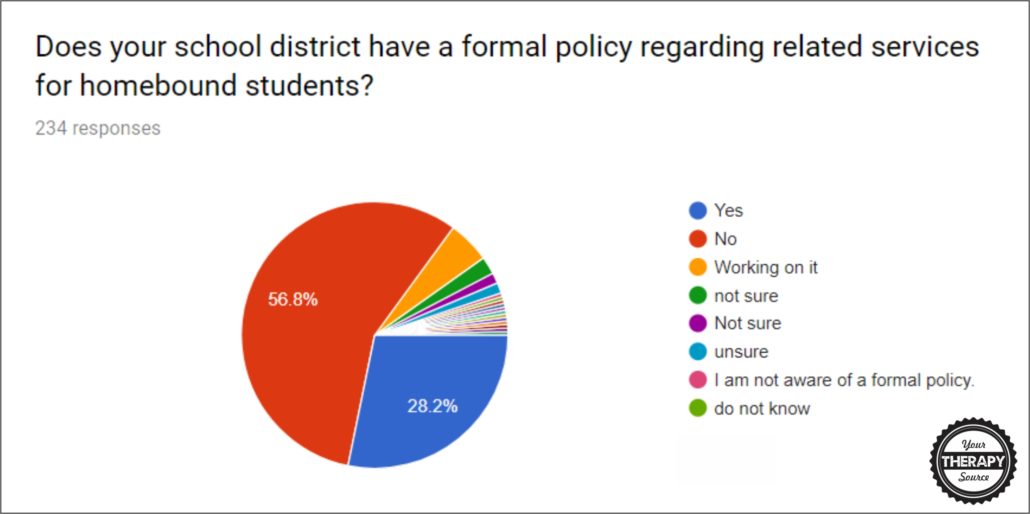
Question #6: Does your school district have a formal policy regarding related services for homebound students?
- 28.2% do have a formal policy regarding related services for homebound students
- 56.8% do not have a formal policy regarding related services for homebound students
Question #7: As a related service provider, what would you change about your school’s practices regarding providing related services to homebound students?
Short Answer Responses:
- Nothing (11)
- consistency (2)
- hire outside contractor to complete these services
- Better define the need for homebound status and have one therapist cover the district instead of different therapists.
- Increased parent and homebound special education teacher knowledge
- Have the student come to public place if medically possible vs. therapist in homes.
- I don’t think there is really anything to change. We typically go out with the teacher and provide support in the area of seating and positioning and/or mobility, typically an hour a month. So far that has worked well.
- I would have a policy in place for therapists to refer to.
- Decrease the reliance on related services without having adequate academic tutoring in place.
- if provided at home needs to be in an effort to relate services to school so that the student can return to school unless the child is medically fragile
- I currently do not have a homebound student. I think criteria for services needs to be clearly stated in a related service policy
- Need to concentrate the number of IEP goals for homebound students and who will implement them.
- OT is related in the school setting. I find that a medical model service is provided in homebound more than accommodations, etc. that might take place in a school setting.
- A policy regarding related services and homebound children is a good idea.
- I would like to see therapists allowed to see the student after the school day and be paid hourly for that service. It is too hard to fit homebound students into an already tight schedule, especially if the service is only going to be temporary.
- There is no one option. Each case is handled individually.
- I would change our practice from direct services (1 or 2x week) to consultation in the home, as many times the student is either too sick for therapies or isn’t motivated to work.
- I would prefer more communication among therapists. This doesn’t happen at all.
- I would formulate a policy about service time and expectations so that they were consistent for all homebound students
- Allow therapist adequate time to add homebound kids to their schedule.
- Have a clear procedure and maybe even a specific team designated to do so
- have a formal policy and more communication with homebound teacher and family about how to hel the student more while homebound.
- Increased communication between parents and staff members as well as clearer guidelines in determining when to put students to home bound status
- remembering to include in IEP meetings
- I would make any homebound student PT consult only.
- compensation should be higher
- improve the efficiency of the process, takes too long to get homebound started
- the teachers who service the homebound students go after school hours for extra pay. Related service providers must go during the school day. It is very difficult to work together.
- Need more formal policies in place, including criteria for discharge/change in service delivery (consult).
- having a policy- reassessing the situation as caseloads change to see if the service would be better outsourced
- The students on homebound have Dr. orders they are medically fragile because the parents wanted it for their children but they would be MUCH BETTER in school with a day full of sensory stimulation and interaction with other students.
- Currently, I only have one on my caseload and she is often too ill for therapies. It is working the way we do it right now.
- our homebound department is totally contracted to teachers after the school day, and most of them are general education teachers, who have no background in working with special needs, cognitively impaired, medically fragile students. Because the teachers are not there until after contracted time, it makes it difficult to interact with them. I would reinstitute teaching positions for these students. The 3-5 year old students do receive services within the school day.
- I think the way we do it works. We assess students and determine if educationally related services are needed based on the student’s needs and what the teacher will be responsible for.
- Some homes/neighborhoods are not safe. It would be great to have a central location for therapy, but there are many variables for this to be successful.
- Would like them to have a set policy rather than set it individually, often based on pushiness of parents and not necessarily on needs of the students
- That the student would have to try to come to school on a shortened day/week after a year of homebound. Most of the homebound students are not that medically fragile and are going on outings with their parents when they are home during the day.
- To have a policy regarding the necessity of school-based related services as part of the homebound instruction. Specifically, how does homebound school-based PT look different than home-care PT services?
- We should not be expected to go into homes that are not safe or are extremely unclean. Our district should come up with another option in those special circumstances.
- There needs to be a clear description and explanation to parents of school-based vs habilitative services.
- I feel that services should be monthly/yearly and primarily consultative because we usually end up delivering services that are more clinically based.
- We have a small percentage of students that receive related services on Homebound.
- We rarely have students that are served in this capacity and usually if they are it is medically fragile children. I do hate that sometimes kids wind up on homebound due to limited communication between doctors and school. In those cases, I wish the doctors would come to meetings or participate by phone.
- No changes, they are a very minimal part of our caseload.
- More consult, less direct. The 2 medically fragile homebound students on my caseload have full-time nurses that know more about them than I ever will. I am not providing skilled service. It is mostly passive range of motion for maintenance which can be taught to caregivers.
- would like to have a formal policy in writing
- Provide more equipment
- Develop consistent guidelines for service type and frequency, discuss equipment, discuss goals, discuss how to best be integrated with teachers versus being more of a medical model
- More defined policy for determining homebound related service provision
- better communication between staff and families on plan of care and progress monitoring
- Should be consultative when going homebound.
- written policy
- Making sure that the IEP is educationally relevant instead of therapy oriented even though the student is receiving services at home.
- Nothing. We take it case by case. We have a general policy, but it can change based on the needs of the student.
- a clearer delineation between medical and educational OT services
- Make more clear-cut guidelines
- Would like more autonomy with goals to reflect the unique needs of a homebound student’s learning needs in their home environment.
- Protocol for frequency of homebound PT services
- Follow the same policy as we have for students who attend school – educational relevance and impact.
- clear guidelines on medical vs. school model
- To have designated therapists service homebound students versus homeschool therapists servicing them, particularly year round.
- have more materials provided
- Teaching staff pay increase. We have many related service providers but not enough teachers for homebound students.
- I think because it is so specific to each student, it works out fairly well. Only issue is sometimes being available so student with primary teacher (ex. if they provide services after school hours).
- When homebound is not for a medical reason but more of a parent preference, district does not push the issue of coming to school
- To not let parents dictate what the student needs, but to let the team as a whole determine what is necessary for the student to benefit from their special education curriculum
- It seems a consultation model would be more appropriate
- They are great using parapros for a monthly home visit instead of sending out professionals for educational tasks
- Improve communication.
- make related services times correlate with instructional time i.e. not give 1 hour of OT if only getting 5 of instruction.
- Have a formal policy regarding related services for homebound students
- district therapists provide services, not contracted therapists
- If the number of homebound students receiving Services Exceed 2, look at the viability of having another therapist provide services for any additional children
- We do have some issues with wanting two staff to go into the home for safety/legal reasons and this is not always approved by administration.
- Add more hours to our schedule to complete homebound services, since it involves more time (driving there and back and the actual service hours) and we both work part time.
- services must be related to the current educational setting. IE home. If the child is able to navigate home environment then PT should be very limited or consult only.
- Improving correlation between homebound therapy and the educational demands as a homebound student.
- if they are medically fragile or unable to attend school then the school-based OT or PT should not be servicing them.
- More consistency in the provision of services
- Have a specific Homebound PT providing the services
- I would like more safety procedures. The school has no idea when or where I go. In today’s world going some places are not safe. It’s also hard when you have a full school day and then go to someone’s house after work hours.
- I am ok with how we do it in my district. I am allowed flexibility to set my schedule and adapt service minutes to best serve the student.
- Our district is doing a good job with it
- Difficulty in scheduling, need to know when school starts
- Clarify policy
- Speed up the process.
- I don’t believe it is appropriate to treat homebound kiddos if the therapist is a school therapist. It should be medically based therapies only. When the kiddo can tolerate school days, then he should get school-based therapy services. We really need to keep the lines clearer.
- We discuss on a case by case basis and I am happy with that
- Make a policy on the appropriateness of serving these students and knowing when to dismiss them from services. Also, educate families and staff on medical vs educational relevance for medically fragile students.
- I think we need a formal policy regarding related services for homebound for medically fragile students that may receive services year long.
- Allow enough time or allow the therapist to do visit after school at contractor’s rate.
- More consistency as to who is eligible.
- It should be more consultative than direct and not just mirror what they would get in a traditional educational setting.
ANSWER OUR CURRENT SURVEY QUESTION
If you need forms and templates to increase communication between school and home check out, School and Home Communication Forms for Therapists.
Therapists, school staff, and parents are all so busy it can be hard to communicate. This collection of forms will save you loads of time. Therapists can review schedules, report on daily or weekly progress, track behavior, review IEP goals, track communication and more. It is suitable for all school-based therapists. Parents can request therapist to complete daily or weekly updates especially beneficial for non-verbal children. FIND OUT MORE.
The post Providing Related Services to Homebound Students Survey Results appeared first on Your Therapy Source.

